Microbial Testing
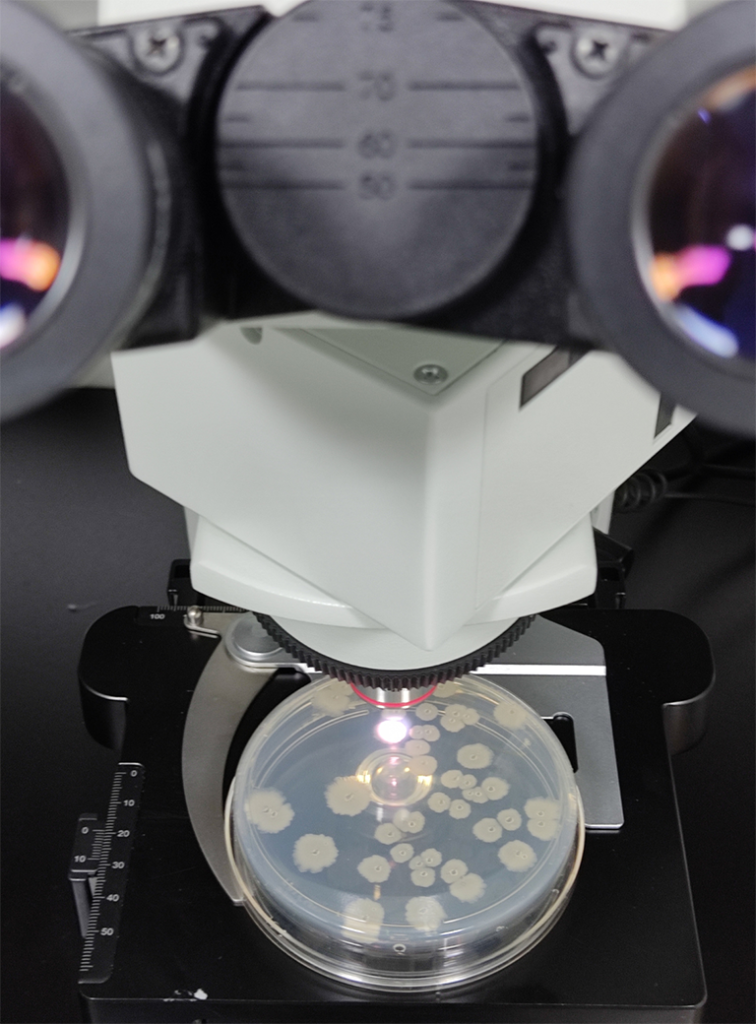
There are many species of bacteria that could potentially be present in your water and food samples. Testing for all of these bacteria would be a time consuming and costly exercise. Generally, we focus our testing on indicator organisms.
Indicator organisms are bacteria that are used to provide evidence of poor hygiene, inadequate processing or post-process contamination of foods. They are often chosen because they are relatively quick and simple to detect. Their absence in water and food provides a degree of assurance that the hygiene and food manufacturing process has been carried out appropriately, whereas their presence usually indicates that a potential problem or failure in the process has occurred.
In addition to testing for indicator organisms, we can perform microbiological testing for specific pathogens on request.
If any of the following pathogens are detected in samples, Queensland Health may need to be notified:
- Salmonella
- Listeria spp.
- Listeria monocytogenes
- Coagulase Positive Staphylococcus



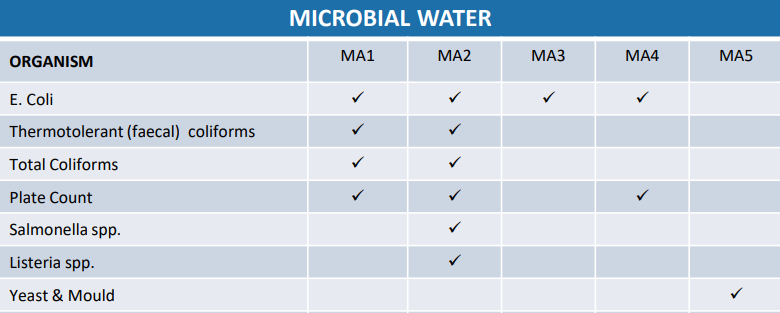
Our Microbial Tests for Water are as follows: